
These Five AI Healthcare Tools May Be the Best Right Now
The options are as staggering as the promise.
Nearly 900 AI health tools have US Food and Drug Administration (FDA) approval, and experts encourage their use to support patient care amid physician shortages and hospital closures.

But just because a tool is FDA-approved does not mean it provides value, said Nigam Shah, PhD, chief data scientist for Stanford Health Care.
You want AI that improves care while lowering costs. “Are we going to make things better or worse?” said Shah, whose team has created AI assessment processes for healthcare systems. “No one’s regulating that.”
To help you wade through the sea of AI options, we asked Shah and other experts to share the AI tools making the biggest impact at their hospitals.
To narrow the list, we prioritized commercially available tools that were mentioned by more than one expert and/or have earned recognition from newly established organizations striving to standardize AI assessment processes, such as the Coalition for Health AI and the Health AI Partnership.
The result is a top-five list of the best AI healthcare tools available now (until something better comes along).
1. LumineticsCore
What it is: AI that diagnoses diabetic retinopathy
Who it’s for: Point-of-care providers, such as optometrists, ophthalmologists, primary care physicians, or endocrinology clinics
Nearly half of people diagnosed with diabetes also have diabetic retinopathy, the leading cause of blindness in the United States — and about half of them don’t know it.
An eye exam can detect the disease, but patients might wait a week or longer for results. The lag discourages follow-up care.
The FDA-approved LumineticsCore is speeding up diagnosis of diabetic retinopathy and macular edema and encouraging more patients to see an ophthalmologist.
After a retinal camera captures images, the system uses an AI-based algorithm and a separate diagnostic algorithm to detect and analyze biomarkers. It provides a diagnosis at the same appointment, so patients can leave with a referral to an ophthalmologist.

Those patients are three times more likely to follow through on the referral than patients diagnosed by a clinician, according to Stanford researchers. LumineticsCore also recently passed Stanford’s assessment, showing “a clear increase in the quality of care,” said Shah.
What makes the tool even more impactful, said Jennifer Goldsack, founder and CEO of DiMe, a non-profit digital medicine organization, is that the company assumes full liability, so providers won’t be held liable if the diagnosis is wrong, and there’s a billing code enabling private insurance reimbursement.
2. Abridge
What it is: An ambient listening tool for clinical notes
Who it’s for: Physicians in any specialty looking to spend less time on the computer

No keyboards. No typing required. That’s how some physicians envision the “hospital of the future,” said Bruce Darrow, PhD, interim chief digital and information officer at the Mount Sinai Health System. Doctors and nurses will speak, and the information will go where it’s needed.
That future is already taking shape with the rise of AI-powered ambient listening tools like Abridge, which originated at the University of Pittsburgh Medical Center, Pittsburgh.
Physicians often catch up on documentation after seeing patients, said Christian Carmody, MBA/MIS, chief technology officer at UPMC. “This helps them do that more efficiently, so they can spend more time taking care of patients.”

According to Abridge’s calculator, a hospital system with 200 physicians can expect to save about 85,000 hours per year (425 hours per doctor) and $1.7 million per year on physician turnover (due to burnout) by using Abridge.
“Almost universally, doctors have told us it frees up time every day that had been spent catching up on administrative notes,” Carmody said.
With patient consent, the tool records interactions and creates a transcript in real time. An AI algorithm grabs key pieces of information to draft clinical notes, which clinicians review before adding to patients’ medical records.
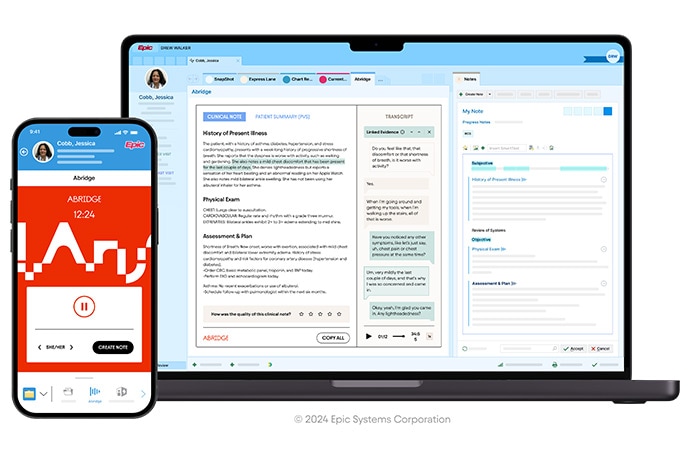
Unique to Abridge is the use of explainable AI: When you highlight parts of the AI-generated note, the tool reveals where in the source transcript the information came from, making it verifiable. It also provides recordings and transcripts to patients.
Designed to work with Epic as well as other electronic health record systems, Abridge is also in use at Emory Healthcare, Yale New Haven Health, Sutter Health, Christus Health, and The University of Chicago.
3. Woebot
What it is: A therapy app aided by machine learning
Who it’s for: Primary care physicians and mental health specialists

Mental health providers are struggling to meet demand. Some patients wait weeks or months to see a specialist after requesting a referral, said Tarun Kapoor, MD, chief digital transformation officer at Virtua Health in Southern New Jersey.
Enter Woebot, a conversational mental health app providing on-demand cognitive behavioral therapy (CBT). The app is available only to patients of partner healthcare institutions, which generally have more than 50 primary care physicians, according to Brad Gescheider, chief commercial officer at Woebot Health. The app has been granted the FDA’s breakthrough device designation, which can help expedite (but not guarantee) FDA approval.
Woebot uses machine learning to understand patients’ messages and delivers pre-written (rather than self-generated) responses. Replies were created by the company’s team of clinicians and writers and hew closely to how clinicians actually respond during interactions with patients.
“It doesn’t fully mimic human conversations with a therapist,” Kapoor said, but programming chatbots with generative AI can be too unpredictable.
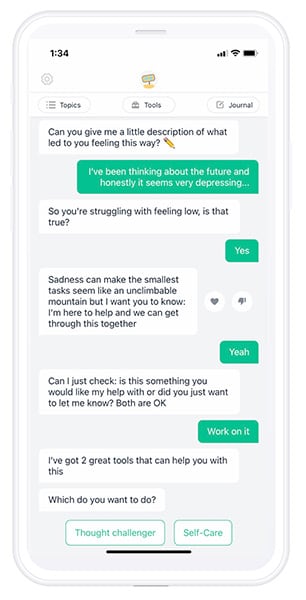
Virtua Health has been prescribing Woebot to a limited population of patients with mild to moderate depression and anxiety, which CBT can help treat. Woebot is provided free to Virtua Health patients. Hospitals and health systems pay a recurring monthly fee based on how many primary care physicians they have.
So far, the app — a two-time MedTech Breakthrough award winner — is proving to be popular and convenient. More than 80% like using it, a typical interaction lasts just 7 minutes, and 77% of interactions occur when providers are off-duty. One insurer impressed with the findings has requested more data, which Kapoor hopes will lead to a reimbursement code.
“We have to show that people are using and getting benefit from the tools we’re recommending and we’re not just adding cost to the system,” Kapoor said.
4. VBrain
What it is: An AI-assisted brain tumor auto-contouring tool
Who it’s for: Radiation oncologists
Before radiation oncologists treat brain tumors, they mark the precise location and mass of each lesion. Correctly identifying the “anatomical part” of each tumor helps clinicians apply radiation more effectively, without damaging surrounding tissue, Shah said. But this manual process, known as tumor contouring, is extremely tedious and time consuming.
“We literally pull up an image, and we’re putting dots and connecting them into an area,” said Shah.
VBrain by Vysioneer speeds up contouring by about 30%, on average, and improves contouring accuracy by 12% compared with manual contouring. Its FDA-approved deep learning algorithm detects the three most common types of brain tumors: Metastasis, meningioma, and acoustic neuroma.
Stanford researchers validated the tool in a study of 100 patients treated with stereotactic radiosurgery, which is preceded by contouring.
“It does 80-90% of the job automatically,” said Shah. “It doesn’t create a materially different outcome, but instead of a human painstakingly drawing something on the image for an hour, they can get it done in 15 minutes.”
5. GI Genius
What it is: AI that detects polyps during colonoscopy
Who it’s for: Gastroenterologists and endoscopists
GI Genius by Medtronic is an AI-powered “back-up camera” FDA approved to help find colon lesions during colonoscopy. Once integrated with existing endoscopy equipment, the tool immediately appears in the endoscopist’s display monitor. It identifies suspected polyps in real time and marks them with green boxes.

“It’s like a second set of eyes,” said Kapoor, of Virtua Health. “The cost is not prohibitively expensive, but look at the benefit.”
GI Genius draws on deep learning algorithms, which can analyze and make predictions about unstructured datasets, including images. In a 2020 study, the tool increased the adenoma (pre-cancerous polyp) detection rate (ADR) by over 14%. Colorectal cancer risk drops 3% for every 1% increase in ADR. In a separate study, it analyzed polyps 82% faster than the endoscopist.
As a bonus, the software generates a report immediately after an endoscopy. “Doctors love that,” Kapoor said. “It’s less time they have to spend doing documentation.”



