The Saga of Aspirin in Preventing Heart Disease
As the pendulum has swung against recommending aspirin for the primary prevention of heart attacks and strokes, clinicians should focus on other ways to help patients avoid cardiovascular events.
A landmark study published in 1988 in the New England Journal of Medicine reported an astonishing 44% drop in the number of heart attacks among US male physicians aged 40-84 years who took aspirin.
Aspirin subsequently became a daily habit for millions of Americans. In 2017, nearly a quarter of Americans over age 40 who did not have cardiovascular disease (CVD) took the drug, and over 20% of those were doing so without a physician’s recommendation.
But in 2018, three studies (ASCEND, ARRIVE, and ASPREE) showed a stunning reversal in the purported benefit, according to John Wong, MD, vice-chair of the US Preventive Services Task Force (USPSTF).

The calculus for taking aspirin appeared to have changed dramatically: The drug decreased the risk for myocardial infarction by only 11% among study subjects, while its potential harms were much more pronounced.
According to Wong, who is also a professor of medicine and a primary care physician at Tufts University School of Medicine in Boston, patients taking low-dose aspirin had a 58% increase in their risk for gastrointestinal bleeding compared with those not on aspirin, as well as a 31% increased risk for intracranial bleeding.
Did aspirin suddenly lose its magic powers in preventing heart attacks? Wong attributed the decline in effectiveness of aspirin in preventing heart attacks to other “primary care interventions that help reduce the cardiovascular disease risk in patients who haven’t had a heart attack or stroke.”
Fewer Americans smoke cigarettes, more realize the benefits of a healthy diet and physical activity, and the medical community better recognizes and treats hypertension. New classes of medications such as statins for high cholesterol are also moving the needle.
But a newer class of drugs may provide a safer replacement for aspirin, according to Muhammad Maqsood, MD, a cardiology fellow at DeBakey Heart and Vascular Center at Methodist Hospital in Houston. P2Y purinoceptor 12 (P2Y12) inhibitors are effective in lowering the risk for heart attack and stroke in patients with acute coronary syndrome or those undergoing elective percutaneous coronary interventions.

“They have shown a better bleeding profile, especially clopidogrel compared to aspirin,” Maqsood said.
However, the findings come from trials of patients who already had CVD, so results cannot yet be extrapolated to primary prevention. Maqsood said the gap highlights the need for clinical trials that evaluate P2Y12 inhibitors for primary prevention, but no such study is registered on clinicaltrials.gov.
Benefits Persist for Some Patients
The new evidence led the USPSTF to publish new guidelines in 2022, downgrading the recommendation for low-dose aspirin use for primary prevention. Previously, the organization stated that clinicians “should” initiate daily low-dose aspirin in adults aged 50-59 years and “consider” its use in adults aged 60-69 years whose 10-year risk for CVD was higher than 10%.
The updated guidelines stated that the decision to initiate low-dose aspirin in adults aged 40-59 years with a greater than 10% risk for CVD “should be an individual one,” based on professional judgment and individual patient preferences. The USPSTF also recommended against the use of aspirin in anyone over the age of 60.
Meanwhile, the American College of Cardiology and American Heart Association also dialed down previously strong recommendations on low-dose aspirin to a more nuanced recommendation stating, “low-dose aspirin might be considered for primary prevention of ASCVD among select adults 40-70 years of age.”
With a varying age limit for recommending aspirin, clinicians may take into consideration several variables.
“Is there a magic age? I don’t think there is,” said Douglas Lloyd-Jones, the former president of the American Heart Association and current chair of the Department of Preventive Medicine and a practicing cardiologist at Northwestern University Feinberg School of Medicine in Chicago.

For a patient over age 60 who is at a high risk for adverse cardiovascular outcomes, is unable to quit smoking, and is not likely to experience problematic bleeding, a clinician might recommend aspirin, Lloyd-Jones said. He said he sometimes also assesses coronary artery calcium to guide his clinical decisions: If elevated (an Agatston score above 100), he might recommend low-dose aspirin.
Lloyd-Jones also reiterated that patients should continue taking low-dose aspirin if they have already experienced a heart attack, stroke, episode of atrial fibrillation, or required a vascular stent.
Unless a patient with established CVD has intractable bleeding, “the aspirin is really for life,” Lloyd-Jones said. Patients who have a stent or who are at high risk for recurrence of stroke are more likely to experience thrombosis, and aspirin can decrease the risk.
“In our cardiology community, we don’t just strictly use the age of 70; the decision is always individualized,” Maqsood said.
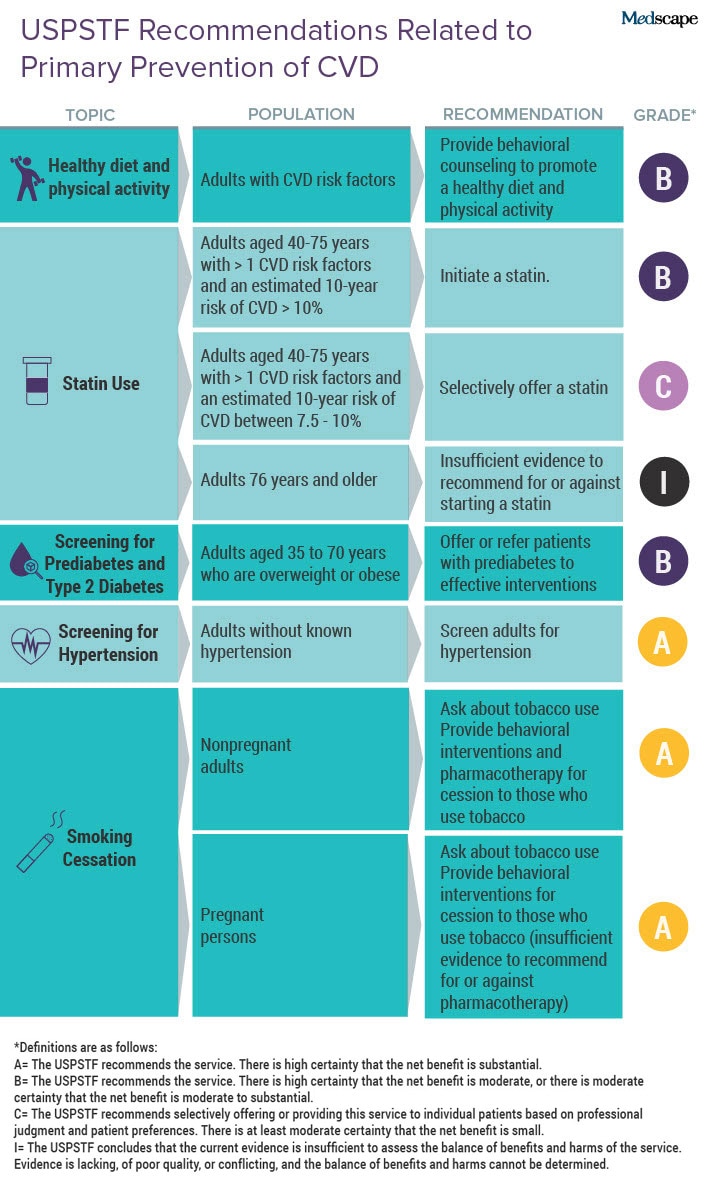
Wong said primary care providers should focus on the USPSTF’s other recommendations that address CVD (Table), such as smoking cessation and screening for hypertension.
“I think our challenge is that we have so many of those A and B recommendations,” Wong said. “And I think part of the challenge for us is working with the patient to find out what’s most important to them.”
Discussing heart attacks and strokes often will strike a chord with patients because someone they know has been affected.
Maqsood emphasized the importance of behavioral interventions, such as helping patients decrease their body mass index and control their hyperlipidemia.
“The behavioral interventions are those which are the most cost-effective without any side effects,” he said.
His other piece of advice is to inquire with younger patients about a family history of heart attacks. Familial hypercholesteremia is unlikely to be controlled by diet and exercise and will need medical therapy.
Lloyd-Jones described the discussions he has with patients about preventing heart attacks as “the most important conversations we can have: Remember that cardiovascular disease is still the leading cause of death and disability in the world and in the United States.”
Wong, Lloyd-Jones, and Maqsood reported no relevant financial relationships.
A former pediatrician and disease detective, Ann Thomas is a freelance science writer living in Portland, Oregon.



